By D. W. G. Kalani Tharanga, JadeTimes News
The virus responsible for mpox, formerly known as monkeypox, was first identified in the late 1950s. Recent years, however, have seen this virus undergo changes that have allowed it to spread more easily among humans, causing concern among global health officials.
Despite its initial discovery in monkeys, mpox is not primarily associated with these animals. The virus was first identified in monkeys during a laboratory experiment in Denmark, but experts like Sagan Friant, an anthropologist at Pennsylvania State University, believe that rodents are the more likely reservoir. Friant has studied mpox in Nigeria for over 15 years and emphasizes that while primates are genetically close to humans, rodent borne diseases are increasingly important in understanding zoonotic threats.
Mpox, a zoonotic disease, has similarities to COVID 19 in its ability to jump from animals to humans and then spread among people. Although it was first identified in 1958, human cases were not documented until 1970. The virus was largely confined to Africa until a 2003 outbreak in the United States, where it spread through infected prairie dogs. In recent years, however, mpox has seen a worrying increase in cases globally, particularly after May 2022, with outbreaks reported in the U.S., Europe, Australia, and Canada.
How Mpox Spreads and Its Impact
Mpox is not as easily transmissible as COVID 19, relying on close physical contact for transmission. It spreads through contact with infectious rashes, lesions, scabs, or bodily fluids. While researchers have detected mpox DNA in semen, it remains unclear whether sexual transmission is a significant route of infection. A study in 2022 found that most cases occurred in men who have sex with men, but this may be due to community spread rather than a unique vulnerability.
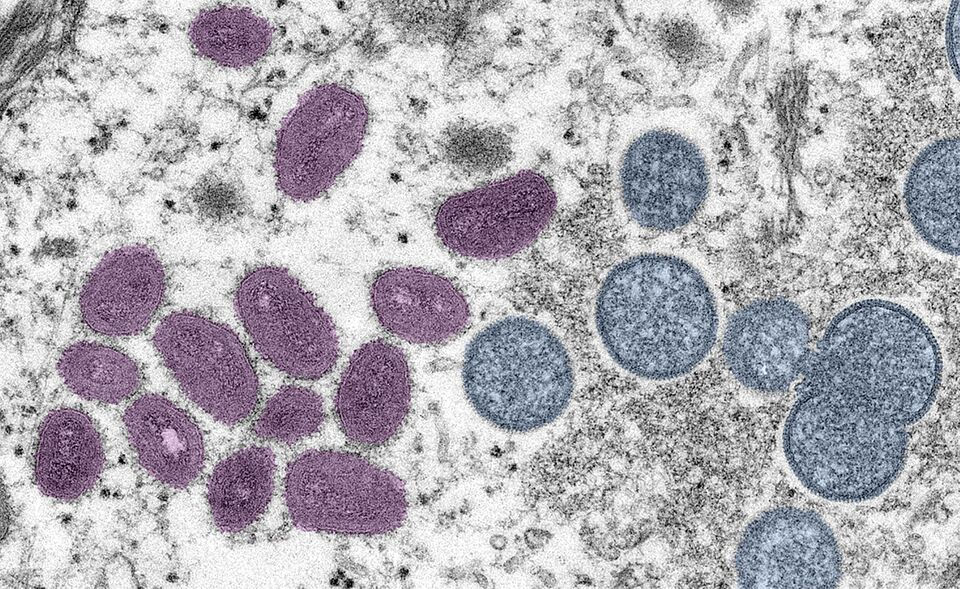
Mpox symptoms are severe and painful, often beginning with flu like symptoms and progressing to a multi stage rash with painful lesions. While the West African strain (clade II) of mpox has a low mortality rate of less than 1%, the Central African strain (clade I) can be far more deadly, with a mortality rate of around 10%.
Despite being a DNA virus, mpox has shown some ability to mutate. Recent outbreaks have identified new variants, like clade Ib in the Democratic Republic of Congo, which spreads more easily among children. These developments have led to renewed concern among health experts, who are closely monitoring the virus for further mutations that could increase its transmissibility or severity.
Global Response and the Need for Vigilance
The global response to mpox has been uneven. Although vaccines developed for smallpox offer protection against mpox, most of these are stockpiled in wealthy nations, leaving endemic regions in Africa at a disadvantage. The Africa Centres for Disease Control and Prevention declared a public health emergency in August 2024 due to the rapid spread of new mpox variants.
The recent mpox outbreaks highlight the need for global cooperation and investment in monitoring zoonotic diseases. As experts warn, mpox is just one of many diseases that could emerge from the interaction between humans and animals, exacerbated by environmental changes. The world must remain vigilant and prepared for the next potential pandemic, ensuring that all regions have the resources and capacity to respond effectively.





























Comentarios